
Corneal neurotization: a narrative review of techniques, outcomes, and surgical considerations
Introduction
Background
Corneal neurotization is a novel surgical technique used to restore corneal sensation in patients with neurotrophic keratopathy, a disorder characterized by decreased or absent corneal sensation. Under normal conditions, corneal innervation serves both sensory and trophic functions for the eye, including initiation of the involuntary blink reflex and regulation of normal epithelial cell function, respectively. The health of the corneal epithelium relies on the delicate relationship between the corneal nerves and the corneal epithelium, which communicate via secreted factors (1). The corneal nerves express factors, including substance C and calcitonin-related gene peptide, that regulate corneal epithelial proliferation and migration. The corneal epithelial cells and keratinocytes, in turn, secrete neuropeptides, neurotrophins, and nerve growth peptides, including nerve growth factor (NGF) and brain-derived neurotrophic factor, which support the health of the corneal nerves (1,2).
In neurotrophic keratopathy, denervation of the ophthalmic division of the trigeminal nerve leads to decreased or absent corneal sensation. Lack of corneal sensation leads to an impaired blink reflex, decreased lacrimal tear secretion, and poor epithelial wound healing, all of which increase the risk for corneal infection, ulceration, perforation, scarring, and vision loss (3).
Rationale and knowledge gap
In the last 15 years, corneal neurotization has emerged as a promising solution to what had previously been an extremely difficult condition to manage. Nevertheless, as new data rapidly emerge, and corneal neurotization procedures gain increasing traction, many questions regarding optimal surgical technique and long-term outcomes remain unanswered.
Objective
In this review, we will synthesize the rapidly evolving field of corneal neurotization as it stands today, with a comprehensive discussion of the management of neurotrophic keratopathy, the practice of corneal neurotization surgery, and important questions that remain. We will begin with an overview of corneal anatomy and innervation, followed by a discussion of neurotrophic keratopathy, its common etiologies, and current management strategies. Next, we will present a review of corneal neurotization techniques and outcomes, as well as key surgical considerations and recommendations for future efforts. We present this article in accordance with the Narrative Review reporting checklist (available at https://aes.amegroups.com/article/view/10.21037/aes-22-33/rc).
Methods
Relevant publications were identified via a PubMed and Google Scholar search using various combinations of the following search terms: “corneal neurotization”, “neurotrophic keratopathy”, “neurotrophic keratitis”, “minimally invasive”, “direct”, “indirect”, “supraorbital”, “supratrochlear”, “infraorbital”, “great auricular”, “sural”, and “lateral antebrachial cutaneous”. A summary of the search strategy and search formulas used are shown in Table 1. Additional papers were identified by reviewing the reference lists of previously identified publications. Special emphasis was placed on publications that described a new technique, examined a unique patient population, compared various techniques, or described important surgical considerations. Publications were chosen based on their relevance to the topic, rather than in a systematic manner. Non-English publications were excluded.
Table 1
| Items | Specification |
|---|---|
| Date of search | 3/1/2022–4/1/2022 |
| Databases and other sources searched | PubMed and Google Scholar |
| Search terms used | Relevant original articles and reviews were retrieved using various combinations of the following search terms: “corneal neurotization”, “neurotrophic keratopathy”, “neurotrophic keratitis”, “minimally invasive”, “direct”, “indirect”, “supraorbital”, “supratrochlear”, “infraorbital”, “great auricular”, “sural”, and “lateral antebrachial cutaneous” |
| Timeframe | 2009–2022 |
| Inclusion and exclusion criteria | Inclusion criteria: research articles and reviews in English about neurotrophic keratopathy and corneal neurotization |
| Exclusion criteria: several publications which were deemed to be of low quality due to insufficient detail | |
| Selection process | Jessica Zhang conducted the selection, all authors discussed the included papers and achieved consensus |
| Any additional considerations, if applicable | Some papers were identified by reviewing the reference lists of previously identified publications |
A review of corneal anatomy and innervation
The cornea is avascular, but also one of the most densely innervated and sensitive tissues in the body (4,5). It serves as a structural barrier against infection and injury, and together with the tear fluid, provides an important refractive surface for the eye (4). The cornea is comprised of five layers, which from most superficial to deep include the corneal epithelium, Bowman‘s membrane, the stroma, Descemet’s membrane, and the endothelium (1).
The cornea receives its innervation from the ophthalmic division of the trigeminal nerve (CN V1). Just before entering the orbit via the superior orbital fissure, the ophthalmic division of the trigeminal nerve gives off the nasociliary nerve, which in turn gives off the long ciliary nerves whose branches ultimately penetrate the cornea in a radial pattern around the limbal circumference (6). These nerve bundles lose their perineurium and myelin sheaths soon after penetrating the corneal stroma at the corneoscleral limbus, branching first into the stromal plexus before piercing Bowman’s membrane and forming a subbasal nerve plexus that supplies the overlying corneal epithelium (1,4). These nerve endings carry information related to nociception, temperature, and pressure sensation, and allow the cornea to respond to various mechanical, chemical, and thermal stimuli (2,5).
Neurotrophic keratopathy
Neurotrophic keratopathy is a relatively rare condition with an estimated prevalence of less than 5/10,000 individuals (3). It is the result of a poorly functioning ophthalmic branch of the trigeminal nerve and can be either congenital or acquired with etiologies varying from infectious, inflammatory, systemic, traumatic, neoplastic, or iatrogenic causes. The more common causes include:
- Herpetic keratitis;
- Local injury via topical anesthetic abuse, chemical burns, and contact lens abuse;
- Diabetes mellitus;
- Multiple sclerosis;
- Intracranial masses;
- Iatrogenic damage from neurosurgical procedures, such as acoustic neuroma removal, and ocular procedures, including cataract extraction, laser in situ keratomileusis (lasik), and vitrectomy (3,5).
Current management options
Neurotrophic keratopathy can be classified into three stages based on severity as described by the Mackie classification system and these various stages in turn govern management (3,7). In stage one, decreased corneal sensation leads to corneal epithelial hyperplasia and irregularities with areas of dried epithelium, superficial punctate keratopathy, corneal edema, and potential superficial neovascularization (3). Management at this stage is aimed at preserving the corneal epithelium and avoiding epithelial breakdown. Treatment includes discontinuation of offending topical medications, especially those with preservatives, treatment of associated underlying conditions (i.e., lagophthalmos from Bell’s palsy or other eyelid abnormalities), and use of preservative-free artificial tears (5). Discontinuing topical medications can be challenging, for instance, as many glaucoma drops, which are crucial to ocular health, are also irritating to the corneal epithelium.
Stage two neurotrophic keratopathy is characterized by recurrent and/or persistent corneal epithelial defects due to impaired epithelial healing. In stage two, treatment includes autologous serum eye drops, therapeutic bandage contact lenses, topical antibiotic drops to prevent infection, and matrix metalloproteinase inhibitors (oral tetracyclines, topical acetylcysteine) to prevent stromal degradation (3). In stage three, these corneal epithelial defects progress to corneal ulcer that can be complicated by stromal involvement, leading to stromal melting and, ultimately, corneal perforation (3).
In more severe cases of stage two, as well as in stage three, neurotrophic keratopathy, both surgical and nonsurgical interventions to temporarily close the eyes can be performed. These include the classic temporary or permanent surgical tarsorrhaphy, as well as a chemically induced upper eyelid ptosis via botulinum toxin injection (3,5). In cases of corneal ulceration, amniotic membrane transplantation (AMT) or conjunctival flap (Gunderson flap) can occasionally preserve the integrity of the ocular surface. In the event of perforation, several options exist, including cyanoacrylate tissue adhesive with therapeutic contact lenses, fibrin glue, corneal patch grafts, and even full corneal transplantation (3). However, corneal transplantation is associated with high levels of recurrence, as lack of trophic factors from the damaged corneal nerves continues to result in poor wound healing and development of epithelial defects (3,5,8).
More recently, topical growth factors and neuropeptides, including substance P, insulin-like growth factor-1, and human NGF (Cenegermin) have been developed to treat neurotrophic keratopathy by restoring the homeostatic signaling that exists between corneal nerves and the corneal epithelium (3,9). While promising, these treatments are costly ($29,665.03 per 8 week treatment) with some patients requiring multiple treatments (10). With insurance companies balking at the price tag, prior authorizations are lengthy, onerous, and coverage can be denied or delayed. Additionally, the substance requires refrigeration/freezing, as well as a complicated application system, making this difficult for those with disabilities or jobs.
Ultimately, these treatment modalities all fail to address the underlying cause of neurotrophic keratopathy, which is corneal denervation. Moreover, the results from current medical and surgical procedures are limited; surgeries like tarsorrhaphy and creation of a conjunctival flap serve to promote corneal epithelial healing and preserve ocular integrity, but at the expense of visual function and poor cosmetic outcomes.
Corneal neurotization
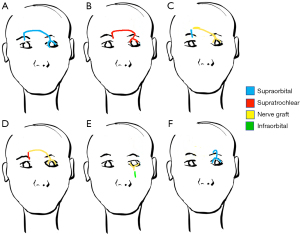
Corneal neurotization is a relatively new surgical technique developed within the last fifteen years to treat neurotrophic keratopathy. Broadly, neurotization is a surgical procedure that reinnervates tissue by transferring healthy sensory or motor nerves from one area of the body to another (11,12). In corneal neurotization, this involves grafting a healthy donor nerve to the junction of the cornea and sclera to restore corneal sensitivity in patients with corneal anesthesia (13). Multiple techniques have been described including direct nerve transfer versus indirect transfer, which requires an interposition nerve graft (Figure 1). When using an interposition graft, the different types and techniques of anastomosis must also be considered: end-to-end versus end-to-side anastomosis, suturing versus gluing, etc.
Patient selection and evaluation
Corneal neurotization was previously reserved for patients refractory to current medical and surgical management, including tarsorrhaphy (13). With improvements in technique and decreases in post-operative recovery time, its applications are widening. Prior to surgical correction with corneal neurotization, patients are evaluated via a comprehensive ocular examination. This typically includes visual acuity, slit-lamp examination, and assessment for corneal sensation. This can be done with a wisp of cotton or more formally via Cochet-Bonnet esthesiometry (14). Using Cochet-Bonnet esthesiometry, corneal sensation can be measured centrally and in all four peripheral quadrants of the anesthetized eye. Normal Cochet-Bonnet scores include measurements of 60 mm and above, with lower numbers correlating with worsening degrees of desensitization (14). Potential donor nerve viability is also measured by assessing sensation, using a cotton wisp, in the regions supplied by the commonly used donor nerves, including the supratrochlear, supraorbital, and infraorbital nerves (11,15-17). Historically, the great auricular nerve (GAN) has been used (18,19), but this has fallen out of favor due to the closer proximity of the orbital nerves mentioned.
Selection of donor nerves
Selection of the donor nerves for neurotization requires both preoperative and intraoperative assessment, and is determined by nerve viability, proximity to the affected cornea, and nerve size/compatibility with an interposition graft (11,17). When possible, ipsilateral donor nerves, either the supraorbital, supratrochlear, or infraorbital nerves are used due to their proximity, followed by contralateral nerves. Some authors have found that the supraorbital nerve has a more consistent anatomy, with a larger diameter compared to the supratrochlear nerve. The infraorbital nerve is slightly less favorable, due to the need for more intricate dissection into the orbit, requiring bone removal. Moreover, transection of the infraorbital nerve has been found to lead to more bothersome sensory loss, particularly in the oral mucosa, compared to the other two. As such, when the infraorbital nerve is used, in conjunction with an interposition graft, it is best to perform end-to-side coaptation to avoid nerve transection and better preserve sensory function (11).
The supratrochlear and supraorbital nerves are branches of the frontal nerve, the largest branch of the ophthalmic division of the trigeminal nerve. After entering the orbit through the superior orbital fissure, the ophthalmic nerve gives off the frontal nerve which then splits into the supratrochlear and supraorbital nerves midway through the orbit. These nerves exit the orbit superiorly with the supraorbital nerve passing through either the supraorbital notch or foramen. They then travel superiorly, beneath the corrugator and frontalis muscles, before piercing through the muscle bellies to reach their intended targets (20). The supratrochlear nerve, the smaller of the two, provides sensory innervation to the skin of the lower forehead and contributes to the sensory innervation of the conjunctiva, while the supraorbital nerve, the larger of the two, supplies a wide area that includes the skin of the upper eyelids, forehead, and scalp (6).
The infraorbital nerve, the terminal branch of the maxillary nerve (CNV2), is another increasingly used donor nerve. It enters the floor of the orbit, via the inferior orbital fissure, before exiting via the infraorbital foramen to provide sensory innervation to the skin and conjunctiva of the lower lid, lateral aspect of the nose, as well as parts of the cheek, upper lip, and oral mucosa (21).
Direct approaches to corneal neurotization
The technique of direct corneal neurotization, whereby a donor nerve is transferred directly to the anesthetized cornea, was first described in 2009 by Terzis et al., who used grafts from contralateral supraorbital and supratrochlear nerves to reinnervate anesthetized corneas in six patients with unilateral facial nerve palsies (22). The technique began with a bicoronal incision across the scalp, followed by dissection of the donor nerves proximal to the supraorbital margin, and tunneling of the nerve branches subcutaneously over the nasal bridge to an eyelid crease incision in the contralateral anesthetic eye. The fascicles of the donor nerves were subsequently dissected free and sutured into the conjunctival sac next to the corneal limbus within the sub-Tenon space. After surgery, patients in the study were followed for an average of 16.3 years, all six showed improvements in corneal sensation by 2.8 years follow up, and most demonstrated improved visual acuity. The drawback here lies in that bicoronal incisions are quite large.
In 2014, Allevi et al. used a similar technique to successfully reinnervate a cornea in a patient with acquired cranial nerve V and VII palsies secondary to removal of a vestibular schwannoma (23). In 2018, Ting et al. also used this technique to treat two patients with neurotrophic keratopathy secondary to cerebellopontine angle meningioma (24).
Ipsilateral nerve transfer
In 2016, Jacinto et al. modified Terzis et al.’s approach to use the ipsilateral supraorbital nerve as a donor nerve, rather than the contralateral one, in a patient with unilateral corneal anesthesia with preserved sensation in the forehead region, suggesting ipsilateral donor nerve viability (25). Rather than a bicoronal incision, this approach allowed for a smaller hemicoronal incision. Following surgery, the patient demonstrated improved corneal sensation as well as improved visual acuity by eight months post-operatively.
Endoscopic contralateral nerve transfer
In 2018, Leyngold et al. described the first case of endoscopic direct corneal neurotization performed on a patient with neurotrophic keratopathy secondary to herpes zoster infection (26). An endoscopic approach, they argued, had the benefit of a smaller incision, quicker recovery time, and fewer proposed complications, including hematoma formation and alopecia. The technique involved creating a small upper eyelid crease incision on the contralateral donor side and dissecting down to the superior orbital rim to expose the supraorbital nerve (Figure 2). Further dissection of the supraorbital nerve, along with subsequent tunneling of the nerve to the recipient eye, were achieved endoscopically via two 1-cm vertical incisions behind the hairline. Two terminal branches of the supraorbital nerve were isolated and passed through a blepharotomy incision to the superior fornix of the affected eye, where the nerve branches were arranged around the cornea in the sub-Tenon’s space. Following surgery, the patient was found to have complete healing of her corneal epithelial defect followed by return of corneal sensation at the three-month follow up visit, though the patient was not followed up beyond this point (26).
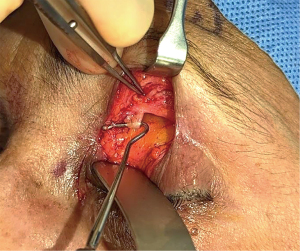
In 2020, Wisely et al. coined this technique a minimally invasive direct corneal neurotization (MIDCN) approach, and described a case series of four patients, who successfully underwent MIDCN using either the ipsilateral or contralateral supraorbital nerve, some using endoscopic guidance and others using only direct visualization (16).
Indirect approaches to corneal neurotization
Sural nerve interposition graft
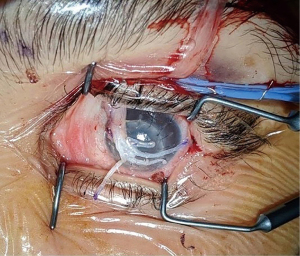
An indirect approach to corneal neurotization, whereby the donor nerve is first coapted to an interposition graft which is then transferred to the anesthetized cornea, was first described in 2014 by Elbaz et al. Their technique used the medial cutaneous branch of the sural nerve as an interposition graft, as sural nerve grafts are commonly used in other surgeries (13,14). The authors argued that using the sural nerve as an interposition graft allows for a smaller initial incision compared to the large bicoronal incision required in open direct neurotization, and that such a technique can be used in cases of bilateral corneal disease (14). In their study, three pediatric patients underwent corneal neurotization. In two of the patients, the surgeons used the contralateral supratrochlear nerve as a donor, while one patient with congenital bilateral corneal anesthesia underwent bilateral corneal neurotization using respective ipsilateral supratrochlear nerves as the sensory donor nerves. To connect the sural nerve to the donor nerve, anastomosis was achieved via end-to-side or end-to-end coaptation of the proximal end of the sural nerve graft to the donor nerve using sutures and fibrin glue. At the distal end, the fascicles of the sural nerve graft were separated, placed around the circumference of the limbus, and sutured to the corneoscleral limbus (Figure 3). Two patients had significantly improved corneal sensation at the six-month visit, while one patient with a history of basal skull fracture regained only partial corneal sensitization by 7.5 months follow-up (14).
Bains et al. utilized a similar technique of sural nerve interposition grafting in four pediatric patients and one adult patient with success as well, primarily using the contralateral supratrochlear nerve as the donor nerve (27). In 2018, Weis et al. demonstrated that the same technique was successful in six adult patients with neurotrophic keratopathy. One patient subsequently had recurrence of his corneal epithelial defect requiring amniotic membrane patch at 17 months post-operatively (28).
Acellular nerve allograft
Leyngold et al. later described successful corneal neurotization in seven patients with neurotrophic keratopathy using a technique similar to that of Elbaz et al., but with acellular nerve allografts (Avance nerve graft, Axogen, Alachua, FL, USA), thus avoiding any donor site morbidity associated with harvesting autologous sural nerve interposition grafts. This resulted in a shorter operative and recovery time than either the endoscopic or coronal approaches previously described. Patients were followed up for a mean period of six months, and all demonstrated improved corneal sensation (11).
GAN interposition graft
In 2018, Benkhatar et al. published their technique using the GAN as an interposition graft rather than the sural nerve (18). The GAN originates from the anterior divisions of the cervical plexus and provides sensation to the earlobe and the fascia of the parotid gland (19). They argue that the GAN is associated with decreased graft morbidity, a shorter operation time, and better end-to-end coaptation with the supratrochlear donor nerve due to better size compatibility of the two (18). Their technique, used in a patient with corneal anesthesia secondary to meningioma resection, involved isolating a 7 cm segment of the ipsilateral GAN within the neck, dissecting and tunneling the contralateral supratrochlear nerve to the affected eye, performing end-to-end coaptation of the two, and lastly dissecting multiple fascicles from the distal GAN graft and securing them under the conjunctiva. Following surgery, the patient demonstrated only slight improvement in corneal sensation at the nine month follow-up, with no improvement in visual acuity or corneal appearance (18).
Great auricular donor nerve with sural nerve interposition graft
In 2019, Jowett et al. developed a new technique whereby they used the ipsilateral GAN as the donor nerve, and harvested the sural nerve as the interposition graft, in two patients with neurotrophic keratopathy. Rather than suture the nerve fascicles to the perilimbal sclera, they also created scleral-corneal tunnel incisions to expedite neurotization. Moreover, they proposed that using the GAN, rather than supratrochlear or supraorbital nerves, as the donor nerve was advantageous because of its relatively larger size and higher axon count, and because it minimized further sensory loss associated with use of branches of the frontal nerve (19). By the nine month follow-up visit, both patients demonstrated improvements in visual acuity and corneal sensation by corneal esthesiometry.
Lateral antebrachial cutaneous nerve interposition graft
In 2019, Bourcier et al. described the first case of corneal neurotization, using an autologous lateral antebrachial cutaneous nerve as the interposition graft, along with the contralateral supraorbital nerve as the donor nerve. Following corneal neurotization, the patient, an adult male with HSV-related neurotrophic keratopathy, had improved corneal sensation and visual acuity with no recurrence of HSV infection by 12 months follow-up (29). A summary of corneal neurotization techniques and their associated advantages and disadvantages is presented in Table 2.
Table 2
| Strategy | Technique | Advantages | Disadvantages |
|---|---|---|---|
| Direct neurotization (donor nerve to anesthetized cornea) | Open contralateral SON and STN: Terzis et al. [2009]; Allevi et al. [2014]; Ting et al. [2018] | First of its kind; however, has generally fallen out of favor | Longer operative time; large bicoronal incision, with higher risk for incision site morbidity and poor cosmetic results; longer recovery time |
| Open ipsilateral SON: Jacinto et al. [2016] | Smaller hemicoronal incision; shorter operative time | Requires intact ipsilateral donor nerves | |
| Minimally invasive contralateral or ipsilateral SON: Leyngold et al. [2018]; Wisely et al. [2020] | Minimally invasive: smaller incisions, quicker recovery time, and fewer complications of hematoma formation and alopecia compared to above | A more difficult dissection of the donor nerve due to smaller incisions, often requiring endoscopic guidance, versus open cases; in cases of contralateral transfer, the length of the donor nerve may be too short to reach the affected cornea, requiring an interposition graft | |
| Short operative time (roughly 60–120 minutes); avoids risk of interposition graft site morbidity and donor nerve-graft coaptation failure associated with interposition grafts; earlier corneal sensation recovery compared to other direct approaches (as early as 2–4 months postoperatively) | |||
| Indirect neurotization (donor nerve to interposition graft to anesthetized cornea) | SN interposition graft to ipsilateral or contralateral SON or STN: Elbaz et al. [2014]; Bainz et al. [2015]; Weis et al. [2018] | Minimally invasive, with no need for scalp incision, reduced risk of alopecia or injury to the facial nerve, and less extensive donor nerve dissection; low risk of morbidity associated with sural nerve grafts | Risk of graft failure and coaptation complications; risk of donor site morbidity associated with sural nerve harvesting; recovery time associated with graft harvesting; requires a larger surgical team in the operating room |
| Acellular interposition allograft to the ipsilateral or contralateral SON, STN, or ION: Leyngold [2019] | Minimally invasive; avoids donor site morbidity associated with harvesting autologous sural nerve; shorter operative time (<90 minutes) compared to all other techniques; potentially smaller surgical team because sural nerve harvesting is not required; earlier corneal sensation recovery compared to other indirect approaches (as early as 3–4 months postoperatively) | Risk of graft failure; cost, availability, and storage requirements associated with acellular allografts | |
| Ipsilateral GAN interposition graft to contralateral STN: Benhkatar et al. [2018] | Minimally invasive; potential to operate in one surgical field, given the proximity of the GAN to the affected cornea | Not commonly performed; the patient recovered only minimal corneal sensation | |
| SN interposition graft to ipsilateral GAN: Jowett [2019] | Minimally invasive; GAN is often still intact in neurotrophic keratopathy; GAN has a higher axonal count than other donor nerves, with a theoretical potential for greater sensory recover; potentially less bothersome to the patient to experience sensory loss in distribution of the GAN (earlobe) rather than in the distribution of SOB or STN (forehead) | Not commonly performed | |
| LABCN interposition graft to contralateral SON: Bourcier et al. [2019] | Minimally invasive; LABCN is purely sensory, with insignificant sensory loss to the patient upon graft harvesting | Not commonly performed |
SON, supraorbital nerve; STN, supratrochlear nerve; ION, infraorbital nerve; SN, sural nerve; GAN, great auricular nerve; LABCN, lateral antebrachial cutaneous nerve.
Outcomes
Corneal neurotization procedures have thus far been relatively successful, with most patients demonstrating improvement in objective corneal sensation by six to ten months follow-up, and as early as two to four months, without recurrence of corneal epithelial defects (14,16,23,24,27). In most patients, Cochet-Bonnet esthesiometry has been the preferred method of measuring corneal sensation before and after surgery. In young children less than 2 years of age, surrogate outcomes have been used to measure successful sensitization, including regression of corneal vascularization, improvement in fluorescein staining, and improvement in corneal clarity (30). In addition to improved corneal sensation, many patients who have undergone corneal neurotization have also experienced improvements in corneal clouding and visual acuity (19,22,23,25,27). In the post-operative period, most patients regained sensation in the distribution of their donor nerves within several months, with the most commonly cited complaints being transient paresthesias or itching in the sensory distribution of the donor nerve, as well as dry eyes requiring daily topical lubrication (18,22).
Moreover, there have been few post-operative complications described thus far. These include one subgaleal hematoma requiring drainage and one neuroma that did not require intervention (22). One patient, who underwent direct neurotization for corneal anesthesia secondary to meningioma resection, had initial improvement in corneal sensation that was not sustained by 2 years follow-up, eventually requiring evisceration with orbital implant due to severe eye pain (24). Another patient with neurotrophic keratopathy secondary to herpes zoster ophthalmicus, who had initial improvement in corneal sensation following indirect neurotization, subsequently developed a corneal epithelial defect requiring AMT 17 months post-operatively (28). Following corneal neurotization, several patients described in this review went on to receive additional eye surgeries, including successful penetrating keratoplasties and cataract surgeries (12,23,28).
More recently, corneal neurotization has been utilized in patients with corneal anesthesia secondary to herpetic keratitis (15,31). Special attention must be paid to donor nerve selection and timing of surgery in these patients, as there is a theoretical potential to spread viral particles during nerve transfer. In one retrospective study of six adult patients with herpetic keratitis, who underwent corneal neurotization, five patients were treated with prophylactic antiviral therapy prior to surgery, and none had clinical evidence of active herpetic disease at the time of surgery. All six experienced improved corneal sensation and visual acuity post-operatively, and no patient had recurrence of herpetic disease, demonstrating that corneal neurotization can be safe and effective in patients with neurotrophic keratopathy secondary to herpetic keratitis (15). In these patients, several cases of recurrent persistent epithelial defects in the post-operative period have been reported, particularly in the first six months, presumably while the corneas were still recovering adequate sensation. These resolved with traditional management, including AMT and bandage contact lenses (15,31).
Corneal reinnervation
Using in vivo confocal microscopy (IVCM), researchers have been able to directly visualize corneal nerves, before and after corneal neurotization, to appreciate evidence of nerve regeneration. IVCM is a non-invasive technique used to obtain high resolution images of the cornea and ocular surface, and has been used in investigations of both systemic and ocular diseases, as well as in studies of corneal reinnervation after corneal transplant and laser refractive procedures (12).
In a study by Fung et al. using IVCM to compare pre- and post-operative corneal innervation in two patients undergoing corneal neurotization, researchers found that the first patient demonstrated a small number of new subbasal nerve fibers at the six month visit, similar to normally innervated corneas, though these new nerves were both less dense and smaller than normal corneal nerves. In the second patient, who subsequently underwent successful corneal transplantation, no subbasal nerve plexus could be discerned on IVCM over one year after corneal transplantation, though several short nerve stumps were found at the junction of the anterior stroma and subbasal layer, which they attributed to the corneal transplantation (12). Ting et al. later used IVCM and histopathological examination to observe corneal nerve regeneration in two patients, who underwent direct neurotization. Similar to Fung et al., they observed in one patient the presence of new, but smaller and less dense, corneal nerves following neurotization compared to normal corneal nerves (24). The other patient initially had improvement in corneal sensation following surgery that was not sustained, and had no evidence of corneal reinnervation by IVCM at 4 years post-operatively. Others have since used IVCM to further confirm the presence of neural regeneration within both the stroma and subbasal layers of the cornea following neurotization (18,19).
Despite evidence of corneal reinnervation demonstrated on IVCM, the actual mechanism behind corneal reinnervation has yet to be fully understood. Two theories have emerged, including corneal reinnervation secondary to direct sprouting from the donor nerve, or native corneal nerve regeneration secondary to the paracrine trophic support supplied by the donor nerve. Using IVCM and histopathological examination of patients’ corneas following direct neurotization, Ting et al. found evidence that regenerated corneal nerves were not continuous with the transplanted donor nerve bundles, suggesting corneal nerve regeneration was secondary to neurotrophic support from the donor nerve, rather than direct sprouting from the donor nerve (24).
However, findings supporting the theory of direct sprouting include observations that in the early stages of the post-operative period, patients who undergo corneal neurotization perceive tactile corneal stimulation as if it were coming from the donor nerve region, suggesting corneal reinnervation via direct sprouting from the donor nerve (14,15). Moreover, in rat models, retrograde labeling of the corneas that underwent neurotization demonstrated that the axons reinnervating the cornea were actually derived from the contralateral infraorbital nerve that was used as a donor nerve, and not preexisting corneal nerves, supporting the theory of direct sprouting from the donor nerve (32). Thus, the direct sprouting theory remains the dominant theory, though further research is still needed to better elucidate the exact pathophysiological mechanism behind corneal reinnervation. Moreover, given support for the theory of direct sprouting, it has been proposed that minimizing the distance between the donor nerve and the anesthetized cornea may theoretically shorten the time to corneal sensitization (33).
Discussion
As corneal neurotization grows in popularity, numerous surgical techniques have been documented, including direct donor to eye versus indirect approaches using an interposition nerve graft. To date, it is unclear if the surgical approach, either direct or indirect neurotization, impacts clinical outcomes.
In a retrospective study of six patients who underwent corneal neurotization for postherpetic neurotrophic keratopathy using both direct and indirect approaches, the authors found no statistical difference in outcomes based on technique (15). A prospective comparative case series of 25 patients who underwent either direct neurotization using the contralateral supraorbital or supratrochlear nerves, or indirect neurotization using a sural nerve interposition graft, likewise found no difference in outcomes (34). In terms of autologous versus allogeneic interposition nerve grafts, one systematic review by Park et al. found no significant difference in outcomes. However, it is difficult to draw conclusions based on existing case reports given the significant heterogenicity of patient ages, anesthesia causes, corneal denervation time, and follow up time (35). Larger, randomized controlled clinical studies with similar patient populations and standardized outcome measures are needed to better compare these various techniques. Anecdotally, however, there has been a draw to using minimally invasive approaches, given their smaller incisions, shorter operative times, and faster recover times (11,16).
Another consideration has been the impact of patient factors, including age, etiology of neurotrophic keratopathy, and duration of the corneal denervation. One systematic review by Wolkow et al. found that none of these factors impacted outcomes (36). In another more recent systematic review by Park et al., researchers found that age was a significant predictor of outcomes, with younger patients experiencing greater improvements in both corneal sensitivity and visual acuity following neurotization. The authors proposed that this may, in part, be due to the greater baseline corneal sensation and subbasal nerve fiber density in eyes of younger patients compared to older ones, leading to a more robust return of corneal innervation following neurotization (35). Moreover, some authors have suggested that surgical intervention earlier in the disease course, based on Mackie staging, may result in greater sensory and visual recovery (15). Thus, it may be more beneficial to perform corneal neurotization earlier in the disease course to improve outcomes.
In terms of visual recovery, the most common limitations to visual acuity improvement have been central corneal scarring, amblyopia, and a history of retinal detachment (11,35). In patients whose visual acuity fails to improve following corneal neurotization, due to irreversible corneal damage, corneal transplantation may be a possible next step, and has been successfully performed in several patients following corneal neurotization. Most subsequent corneal transplantations have been performed at least a year following neurotization, though a successful case of simultaneous direct corneal neurotization and corneal transplantation has been described (16,33).
Lastly, despite advances in corneal neurotization, recent advances in the medical management of neurotrophic keratopathy, particularly the FDA approved recombinant topical human NGF (rhNGF), Cenegermin, have emerged as a possible alternative or addition to surgical management. However, while clinical trials of rhNGF have shown it to be effective at improving corneal epithelial health and healing, rhNGF has not been shown to improve corneal sensation. Moreover, recurrence rates of corneal epithelial defects with topical rhNGF may be higher than those seen with corneal neurotization (37). Nevertheless, topical rhNGF agents like Cenegermin may be an appropriate option in those who are poor surgical candidates, or as an adjuvant therapy in addition to corneal neurotization. More research is needed to compare medical and surgical management of neurotrophic keratopathy, and to study the effects of combination therapies.
Conclusions
Corneal neurotization has emerged within the last fifteen years as a promising approach to managing neurotrophic keratopathy, a debilitating and difficult-to-treat condition. In studies so far, corneal neurotization has been shown to restore corneal sensation, improve corneal epithelial health, and improve visual acuity. Corneal neurotization remains the only option to date that addresses the underlying pathophysiology of neurotrophic keratopathy by reinnervating anesthetized corneas. Future efforts are needed to evaluate the various corneal neurotization techniques in larger sample sizes of patients, study long term corneal neurotization outcomes, and compare surgical intervention with emerging medical therapies.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Joann Kang and Roy S. Chuck) for the series “Ocular Surface Reconstruction/Transplantation” published in Annals of Eye Science. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://aes.amegroups.com/article/view/10.21037/aes-22-33/rc
Conflicts of Interest: Both authors has completed the ICMJE uniform disclosure form (available at https://aes.amegroups.com/article/view/10.21037/aes-22-33/coif). The series “Ocular Surface Reconstruction/Transplantation” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sacchetti M, Lambiase A. Neurotrophic factors and corneal nerve regeneration. Neural Regen Res 2017;12:1220-4. [Crossref] [PubMed]
- Yang AY, Chow J, Liu J. Corneal Innervation and Sensation: The Eye and Beyond. Yale J Biol Med 2018;91:13-21. [PubMed]
- Sacchetti M, Lambiase A. Diagnosis and management of neurotrophic keratitis. Clin Ophthalmol 2014;8:571-9. [PubMed]
- DelMonte DW, Kim T. Anatomy and physiology of the cornea. J Cataract Refract Surg 2011;37:588-98. [Crossref] [PubMed]
- Dua HS, Said DG, Messmer EM, et al. Neurotrophic keratopathy. Prog Retin Eye Res 2018;66:107-31. [Crossref] [PubMed]
- Shankland WE. The trigeminal nerve. Part II: the ophthalmic division. Cranio 2001;19:8-12. [Crossref] [PubMed]
- Mackie IA. Neuroparalytic keratitis. Current Ocular Therapy 1995:452-4.
- Jhanji V, Young AL, Mehta JS, et al. Management of corneal perforation. Surv Ophthalmol 2011;56:522-38. [Crossref] [PubMed]
- Yamaguchi T, Turhan A, Harris DL, et al. Bilateral nerve alterations in a unilateral experimental neurotrophic keratopathy model: a lateral conjunctival approach for trigeminal axotomy. PLoS One 2013;8:e70908. [Crossref] [PubMed]
- Oxervate Prices and Oxervate Coupons. GoodRx. Retrieved April 25, 2022. Available online: https://www.goodrx.com/oxervate
- Leyngold IM, Yen MT, Tian J, et al. Minimally Invasive Corneal Neurotization With Acellular Nerve Allograft: Surgical Technique and Clinical Outcomes. Ophthalmic Plast Reconstr Surg 2019;35:133-40. [Crossref] [PubMed]
- Fung SSM, Catapano J, Elbaz U, et al. In Vivo Confocal Microscopy Reveals Corneal Reinnervation After Treatment of Neurotrophic Keratopathy With Corneal Neurotization. Cornea 2018;37:109-12. [Crossref] [PubMed]
- Kolseth CM, Charlson ES, Kossler AL. Corneal Neurotization: A Surgical Treatment for Neurotrophic Keratopathy. J Neuroophthalmol 2020;40:e11-2. [Crossref] [PubMed]
- Elbaz U, Bains R, Zuker RM, et al. Restoration of corneal sensation with regional nerve transfers and nerve grafts: a new approach to a difficult problem. JAMA Ophthalmol 2014;132:1289-95. [Crossref] [PubMed]
- Kim JS, Rafailov L, Leyngold IM. Corneal Neurotization for Postherpetic Neurotrophic Keratopathy: Initial Experience and Clinical Outcomes. Ophthalmic Plast Reconstr Surg 2021;37:42-50. [Crossref] [PubMed]
- Wisely CE, Rafailov L, Cypen S, et al. Clinical and Morphologic Outcomes of Minimally Invasive Direct Corneal Neurotization. Ophthalmic Plast Reconstr Surg 2020;36:451-7. [Crossref] [PubMed]
- Sweeney AR, Wang M, Weller CL, et al. Outcomes of corneal neurotisation using processed nerve allografts: a multicentre case series. Br J Ophthalmol 2022;106:326-30. [Crossref] [PubMed]
- Benkhatar H, Levy O, Goemaere I, et al. Corneal Neurotization With a Great Auricular Nerve Graft: Effective Reinnervation Demonstrated by In Vivo Confocal Microscopy. Cornea 2018;37:647-50. [Crossref] [PubMed]
- Jowett N, Pineda Ii R. Corneal neurotisation by great auricular nerve transfer and scleral-corneal tunnel incisions for neurotrophic keratopathy. Br J Ophthalmol 2019;103:1235-8. [Crossref] [PubMed]
- Janis JE, Hatef DA, Hagan R, et al. Anatomy of the supratrochlear nerve: implications for the surgical treatment of migraine headaches. Plast Reconstr Surg 2013;131:743-50. [Crossref] [PubMed]
- Shafique S, Das JM. Anatomy, Head and Neck, Maxillary Nerve. StatPearls. Treasure Island (FL): StatPearls Publishing, 2022.
- Terzis JK, Dryer MM, Bodner BI. Corneal neurotization: a novel solution to neurotrophic keratopathy. Plast Reconstr Surg 2009;123:112-20. [Crossref] [PubMed]
- Allevi F, Fogagnolo P, Rossetti L, et al. Eyelid reanimation, neurotisation, and transplantation of the cornea in a patient with facial palsy. BMJ Case Rep 2014;2014:bcr2014205372. [Crossref] [PubMed]
- Ting DSJ, Figueiredo GS, Henein C, et al. Corneal Neurotization for Neurotrophic Keratopathy: Clinical Outcomes and In Vivo Confocal Microscopic and Histopathological Findings. Cornea 2018;37:641-6. [Crossref] [PubMed]
- Jacinto F, Espana E, Padilla M, et al. Ipsilateral supraorbital nerve transfer in a case of recalcitrant neurotrophic keratopathy with an intact ipsilateral frontal nerve: A novel surgical technique. Am J Ophthalmol Case Rep 2016;4:14-7. [Crossref] [PubMed]
- Leyngold I, Weller C, Leyngold M, et al. Endoscopic Corneal Neurotization: Technique and Initial Experience. Ophthalmic Plast Reconstr Surg 2018;34:82-5. [Crossref] [PubMed]
- Bains RD, Elbaz U, Zuker RM, et al. Corneal neurotization from the supratrochlear nerve with sural nerve grafts: a minimally invasive approach. Plast Reconstr Surg 2015;135:397e-400e. [Crossref] [PubMed]
- Weis E, Rubinov A, Al-Ghoul AR, et al. Sural nerve graft for neurotrophic keratitis: early results. Can J Ophthalmol 2018;53:24-9. [Crossref] [PubMed]
- Bourcier T, Henrat C, Heitz A, et al. Lateral Antebrachial Cutaneous Nerve as Autologous Graft for Mini-Invasive Corneal Neurotization (MICORNE). Cornea 2019;38:1029-32. [Crossref] [PubMed]
- Sepehripour S, Lloyd MS, Nishikawa H, et al. Surrogate Outcome Measures for Corneal Neurotization in Infants and Children. J Craniofac Surg 2017;28:1167-70. [Crossref] [PubMed]
- Lin CH, Lai LJ. Herpetic Corneal Keratopathy Management Using Ipsilateral Supratrochlear Nerve Transfer for Corneal Neurotization. Ann Plast Surg 2019;83:553-7. [Crossref] [PubMed]
- Catapano J, Antonyshyn K, Zhang JJ, et al. Corneal Neurotization Improves Ocular Surface Health in a Novel Rat Model of Neurotrophic Keratopathy and Corneal Neurotization. Invest Ophthalmol Vis Sci 2018;59:4345-54. [Crossref] [PubMed]
- Liu CY, Arteaga AC, Fung SE, et al. Corneal neurotization for neurotrophic keratopathy: Review of surgical techniques and outcomes. Ocul Surf 2021;20:163-72. [Crossref] [PubMed]
- Fogagnolo P, Giannaccare G, Bolognesi F, et al. Direct Versus Indirect Corneal Neurotization for the Treatment of Neurotrophic Keratopathy: A Multicenter Prospective Comparative Study. Am J Ophthalmol 2020;220:203-14. [Crossref] [PubMed]
- Park JK, Charlson ES, Leyngold I, et al. Corneal Neurotization: A Review of Pathophysiology and Outcomes. Ophthalmic Plast Reconstr Surg 2020;36:431-7. [Crossref] [PubMed]
- Wolkow N, Habib LA, Yoon MK, et al. Corneal Neurotization: Review of a New Surgical Approach and Its Developments. Semin Ophthalmol 2019;34:473-87. [Crossref] [PubMed]
- Bonini S, Lambiase A, Rama P, et al. Phase II Randomized, Double-Masked, Vehicle-Controlled Trial of Recombinant Human Nerve Growth Factor for Neurotrophic Keratitis. Ophthalmology 2018;125:1332-43. [Crossref] [PubMed]
Cite this article as: Zhang J, Barmettler A. Corneal neurotization: a narrative review of techniques, outcomes, and surgical considerations. Ann Eye Sci 2023;8:7.


